1000 AI Algorithms in Medical Imaging – Thoughts for Tech Entrepreneurs (2 of 5)
In the first article, I described the number of findings and conditions radiologists typically work with on a daily basis and why I believe we need to go from about 70 to 1000 algorithms to make significant progress in applying AI to medical imaging. If you missed it, you can read it here.
And in case you need more convincing, you can take a look at this video and start at 1:06 and watch about 10 minutes to see the vast number of problems to solve. Thank you to ACR and Keith Dreyer.
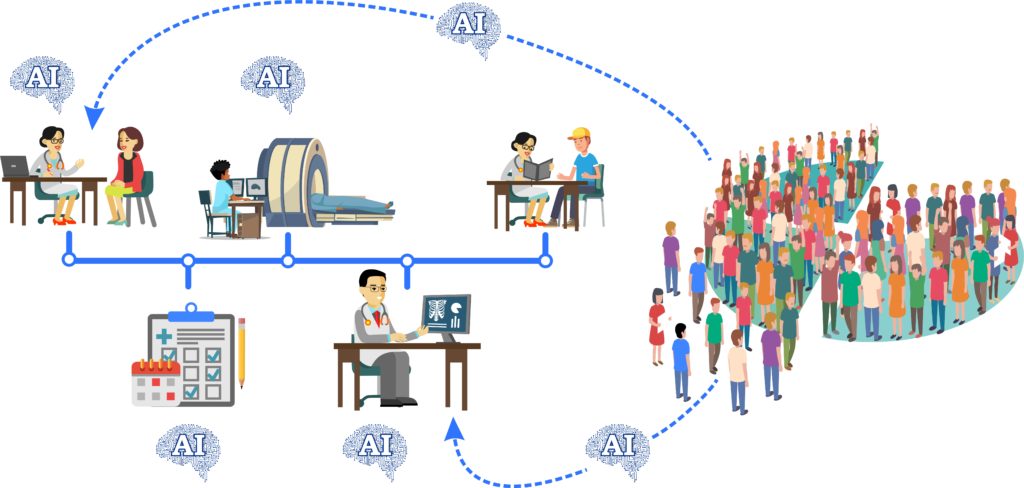
In this article I am going to explain the process, literally walk you through what happens from patient/provider encounter to interpreting the imaging. Gemba is a term in Lean Manufacturing which means ‘walk through’ and I think there is benefit to shining a light on each step to really clarify and find opportunities. This will also help understand where data is collected and where it is (not cleanly) stored. I will place an (AI⚡️) at a few places where data could be curated and data science and/or an algorithm could be employed. I bet you can find a few more places you’d like to place (AI⚡️) as well.
Let’s step back and remember the medicine is in the dark ages when it comes to regular business intelligence. We create so much data exhaust we don’t even know where to begin.
So let’s start at the beginning.
A patient is in a provider’s office with a problem that is concerning to them. Since it was probably difficult to make the appointment (AI⚡️) the patient may have more than one question but for this example let’s just pick one, low back pain.
The provider listens and asks questions (AI⚡️) of this 40 year old man: What is the context? Was there trauma? How long has the pain been there? Anything make it worse? Is there something different about the pain that brought you in today? Pain anywhere else? It turns out this pain has been there for about a year and slowly getting worse and shooting down his right leg. Over the year, the leg pain has been getting more frequent and extending further down, now to his right knee. He is a hard working guy and remembers lifting a heavy tool box about the time it started. (AI⚡️)
The provider is continuously going through a list of reasons for back pain, starting with true emergencies, trauma or infection for example, and after the clinician is convinced that it is not emergent, they settle on the most likely problem is a bulging disk in the lower spine pressing on the nerve that goes to the right leg. (AI⚡️) Based on decision support literature, the best way to confirm this suspicion is with an MRI of the lumbar spine without contrast. This type of support is not universally electronically available within the electronic medical record so providers may need to use a browser search to find the best imaging test. (AI⚡️)
In the electronic medical record, the provider can place an order for the MRI. Usually this is a selectable menu item and many times the provider needs to retype the patients information in the order so the radiologist can have all of the pertinent information to help while making a report for the scan. Sometimes these orders are literally printed on papers and then scanned at radiology departments. Ideally when everything is connected properly, there is a Radiology Information System (RIS) which collects some data to pass to the radiology department. (AI⚡️)
There are usually a few steps before scheduling, a common one is insurance approval. (AI⚡️) Once approved, the patient can call to schedule the exam. Requesting arrival 15 minutes early is common to fill out some forms on paper. With a pen. These forms are critical to gather information to be sure there is no danger to the patient prior to the MRI, like is there any worrisome metal inside the patient. (AI⚡️) One example for someone who works with metal and could possibly have tiny metal shavings in their eyes. The magnet in an MRI is very strong and if there were big enough pieces of metal the magnet could move them or pull them out. So in this case, the patient was not sure so he had an x-ray of his face and eyes to see if there are any concerning metallic fragments. It was clear, no metal and he is good to go.
He takes all metal objects out of his pockets and verified with a metal detector and goes into the scanner room with hearing protection. The technologist properly places them on the table (AI⚡️) with a device called coil sometimes placed over their abdomen to help create the images.
The technologist had likely preselected the proper controls on the MRI workstation. (AI⚡️) There are specific protocols for every MRI and they are all very specific to be sure to capture the correct information. A single MRI exam will include many scans which means the patient goes in and out of the middle of the scanner many times and this can take 20-45 minutes or longer depending on how much information is needed.
The technologist looks at all of the images from all of the scans, which may be in the hundreds, to be sure the quality is appropriate. If a patient moves, just a little bit, the images appear very blurry and sometimes need to be repeated. (AI⚡️) Once the patient exits the scanner room, the technologist sends the images from the computer connected to the MRI machine to the computer system where radiologists look at the images, called PACS (Picture Archive and Communication System).
This MRI exam will appear on the radiologist’s list similar to an email inbox. There are likely many on this list and exams from the emergency department or ICU are usually pushed to the top of the list (AI⚡️) and when those are done, the radiologist will work on all of the other CT scans, ultrasounds, x rays and MRI scans.
When this patient’s MRI is clicked open, all of the different scans, called sequences, are displayed on a large computer monitor and they should be arranged properly which is called a hanging protocol. (AI⚡️) A long time ago, x-rays used to be “hung” for radiologists to read them. Even though it is digital, we still use that term.
The radiologist scrolls through all of the images, in all of the sequences while speaking into a microphone connected to a voice recognition system to create the report. If there are things to measure, that is done by selecting a ruler and clicking and dragging on the area. (AI⚡️) In this patient, for example, let’s say the disc that was pressing on the nerve to the leg measured 5 mm, that would be added to the report, in the proper section. (AI⚡️) The sections are usually nicely organized in a premade template and each part is filled in. Bones, muscles, vessels, spinal cord and each disc, level by level from L1-L2 to L5-S1. (AI⚡️)
Once the report is completed, it is digitally signed by the radiologist and sent to the electronic health record for the ordering provider to see the report and make a plan with the patient. If there was a concerning finding, the radiologist would call the ordering provider so they could call the patient and take care of it appropriately. (AI⚡️)
How many other places in this scenario could have used (AI⚡️) ?
And remember, this is just radiology. And there are similar workflows for labs, specialist referrals, dietary or physical therapy consultations or pharmacy. Digging in on each of these pain points are opportunities in and of themselves. The tedious task of walking through the process is critical to finding pain points to address in the market and this is why a person with clinical domain expertise is needed on the team.
Article 3 will explain a clinical scenario and questions to keep in mind while looking to build, fund and sell a platform.

